What is insulin resistance and how does it contribute to Type 2 diabetes?
Insulin resistance is a pivotal factor in the development of Type 2 diabetes, a condition characterized by high blood sugar levels. Let's delve into what insulin resistance entails and how it contributes to the onset of Type 2 diabetes.
What is Insulin Resistance?
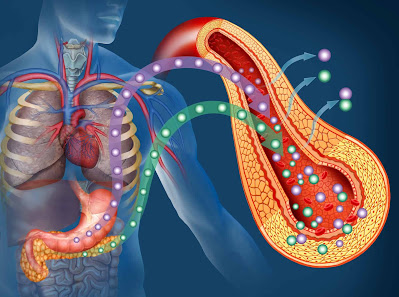
Insulin, produced by the pancreas, is a hormone responsible for regulating blood sugar levels in the body. It facilitates the uptake of glucose by cells, where it is used for energy production. However, in individuals with insulin resistance, cells become less responsive to the action of insulin.
As a result, glucose uptake is impaired, leading to elevated blood sugar levels. Insulin resistance often precedes the diagnosis of Type 2 diabetes and is a hallmark feature of the condition.
How Insulin Resistance Contributes to Type 2 Diabetes
Insulin resistance sets off a cascade of metabolic changes that ultimately contribute to the development of Type 2 diabetes. To compensate for the decreased sensitivity of cells to insulin, the pancreas ramps up insulin production, attempting to maintain normal blood sugar levels. Initially, this compensatory mechanism may succeed in preventing hyperglycemia.
However, over time, the pancreas becomes overwhelmed by the demand for insulin, leading to a decline in its ability to produce adequate amounts of the hormone. As a result, blood sugar levels rise, eventually reaching levels diagnostic of Type 2 diabetes.
Moreover, insulin resistance is associated with various metabolic abnormalities, including dyslipidemia (abnormal lipid levels) and hypertension (high blood pressure), further increasing the risk of cardiovascular complications in individuals with Type 2 diabetes.
Risk Factors and Causes of Insulin Resistance
Several factors contribute to the development of insulin resistance, increasing the risk of Type 2 diabetes. One of the primary risk factors is obesity, particularly excess abdominal fat. Adipose tissue, especially visceral fat, releases inflammatory cytokines and adipokines, which interfere with insulin signaling, promoting insulin resistance.
Additionally, physical inactivity and a sedentary lifestyle are significant contributors to insulin resistance. Regular exercise enhances insulin sensitivity, whereas a lack of physical activity promotes insulin resistance. Genetics also play a crucial role in insulin resistance susceptibility.
Certain gene variants, such as those affecting insulin receptor function or intracellular signaling pathways, can predispose individuals to insulin resistance. Furthermore, aging is associated with a natural decline in insulin sensitivity, increasing the risk of insulin resistance and Type 2 diabetes.
Hormonal imbalances, such as elevated levels of cortisol (a stress hormone) or decreased levels of adiponectin (an insulin-sensitizing hormone), can also impair insulin action. Chronic stress, characterized by prolonged activation of the body's stress response system, can exacerbate insulin resistance.
Other factors, including poor dietary choices (e.g., excessive consumption of refined carbohydrates and sugary foods), smoking, and sleep deprivation, can further contribute to insulin resistance.
Symptoms and Complications of Insulin Resistance
Insulin resistance often develops silently, without causing noticeable symptoms in its early stages. However, as the condition progresses, individuals may experience symptoms related to elevated blood sugar levels, such as increased thirst, frequent urination, fatigue, and blurred vision.
Moreover, insulin resistance is a key driver of metabolic syndrome, a cluster of conditions including abdominal obesity, dyslipidemia, hypertension, and impaired glucose metabolism, which significantly increases the risk of cardiovascular disease and Type 2 diabetes.
Left untreated, insulin resistance can lead to the development of Type 2 diabetes, characterized by chronic hyperglycemia and an increased risk of diabetes-related complications, such as heart disease, stroke, kidney disease, neuropathy, and retinopathy. Therefore, early detection and intervention are crucial in preventing or delaying the progression from insulin resistance to Type 2 diabetes and its associated complications.
Diagnosis of Insulin Resistance
Diagnosing insulin resistance typically involves a combination of medical history, physical examination, and laboratory tests. Healthcare providers may inquire about risk factors such as family history of diabetes, obesity, and sedentary lifestyle during the medical history assessment.
Physical examination may include measurements of body weight, waist circumference, and blood pressure, as well as an evaluation of signs associated with insulin resistance, such as acanthosis nigricans (a skin condition characterized by dark, velvety patches). Laboratory tests are used to assess fasting insulin levels, fasting glucose levels, and sometimes hemoglobin A1c levels.
Elevated fasting insulin levels, along with normal or mildly elevated fasting glucose levels, indicate insulin resistance. Additionally, oral glucose tolerance tests (OGTT) may be conducted to evaluate how the body responds to a glucose challenge over time. An OGTT involves fasting overnight, followed by consumption of a glucose solution and periodic blood sugar measurements over several hours.
Abnormal glucose tolerance curves during an OGTT can further confirm the presence of insulin resistance. Early detection and diagnosis of insulin resistance are crucial for implementing appropriate interventions to prevent or delay the progression to Type 2 diabetes and its associated complications.
Treatment and Management of Insulin Resistance
The primary goals of managing insulin resistance are to improve insulin sensitivity, regulate blood sugar levels, and reduce the risk of developing Type 2 diabetes and cardiovascular disease. Lifestyle modifications play a central role in the treatment of insulin resistance.
These include adopting a healthy diet rich in fiber, fruits, vegetables, and whole grains, while limiting intake of refined carbohydrates, sugary foods, and saturated fats. Regular physical activity is essential for enhancing insulin sensitivity and promoting weight loss. Aerobic exercise, resistance training, and flexibility exercises can all contribute to improving insulin sensitivity and metabolic health.
Additionally, achieving and maintaining a healthy weight through calorie control and portion management is crucial for managing insulin resistance. In some cases, medications may be prescribed to help improve insulin sensitivity or regulate blood sugar levels. These may include insulin-sensitizing drugs such as metformin, thiazolidinediones, or medications that promote weight loss.
Close monitoring of blood sugar levels, regular medical check-ups, and ongoing support from healthcare providers are essential components of long-term management for individuals with insulin resistance.
By implementing comprehensive lifestyle changes and medical interventions, individuals with insulin resistance can effectively manage their condition and reduce their risk of developing Type 2 diabetes and its associated complications.
Conclusion:
Insulin resistance is a critical precursor to Type 2 diabetes, significantly impacting metabolic health and increasing the risk of cardiovascular complications. Early detection and proactive management are key to preventing the progression to diabetes and associated complications.
To learn more about insulin resistance, Type 2 diabetes, and how to manage these conditions effectively, consider exploring reputable sources such as:
1. American Diabetes Association (ADA):(https://www.diabetes.org)
2. Centers for Disease Control and Prevention (CDC): www.cdc.gov/diabetes
3. Mayo Clinic: www.mayoclinic.org/diseases-conditions/type-2-diabetes
4. National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): [www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes]
By staying informed and proactive, individuals with insulin resistance can take control of their health and reduce their risk of developing Type 2 diabetes and its complications.



Comments
Post a Comment
Share your views