Diabetes Reversed In Mice After Scientists Hacked Human Cells To Produce Insulin
Without the hormone insulin, blood glucose levels would rise too high, leading to diabetes and all of its problems. Type 1 diabetes, which affects an estimated 1.6 million Americans, is brought on by an autoimmune response that kills the beta cells in the pancreas.
Numerous additional Americans, at least a few million, suffer from severe type 2 diabetes and lack enough beta cells. Currently available therapies for these conditions include manual and wearable-pump insulin injections, which have a number of disadvantages including discomfort, potentially ineffective glucose management, and the requirement to wear bulky equipment.
Case study
Researchers from Weill Cornell Medicine in the US conducted an experiment that showed transplanting gastric insulin-secreting (GINS) cells could cure mice of diabetes.
As a typical response to increased blood sugar levels, pancreatic beta cells release the hormone insulin. These tissues suffer harm or degenerate in diabetics, impairing their capacity to transport glucose into cells for energy.
Despite not being beta cells, GINS cells can perform beta cells' functions. The gut is rich in stem cells, which may differentiate into a wide variety of cell types and multiply swiftly. It is hoped that diabetes patients' own gut stem cells will be converted into GINS cells, reducing the possibility of rejection.
According to Joe Zhou, an associate professor of regenerative medicine at Weill Cornell Medicine in New York, the stomach produces its own hormone-secreting cells, and stomach cells and pancreatic cells are adjacent in the embryonic stage of development, so in that sense it isn't completely surprising that gastric stem cells can be so easily transformed into beta-like insulin-secreting cells.
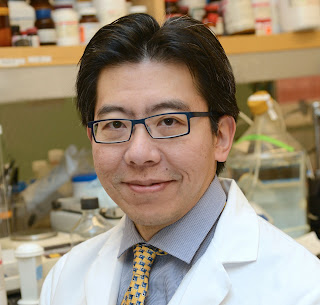 |
| Joe Zhou, an associate professor of regenerative medicine at Weill Cornell Medicine in New York |
Over the years, scientists have made numerous unsuccessful attempts to make something similar to work. For the purpose of this study, the scientists activated three distinct proteins in the cells that regulate gene expression in a precise order to cause a transformation into GINS cells.
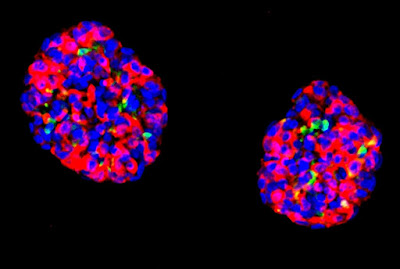
The reconfiguration procedure is very effective, as the cells displayed glucose sensitivity after being cultivated in organoids, which are condensed collections of cells. The mice's diabetes may subsequently be shown to have long-lasting repercussions.
The researchers assert that the technique of creating GINS cells from stomach cells is not overly difficult. These new organoids can survive after transplantation for several months and it only takes a few days for it to happen, according to their testing.
The researchers write in their paper that "Gastric insulin-secreting (GINS) organoids exhibited glucose responsiveness 10 days after induction." They released human insulin, cured diabetes in mice, and were stable following transplantation for the six months we monitored them.
In order to control blood glucose, the hormone insulin is essential. Without enough amounts, we are at danger for several health issues. Diabetes affects millions of individuals worldwide, most of whom use insulin injections to help control blood sugar levels.
Research Study Conclusion
Although this method is still in its infancy, it would allow the body to once again regulate insulin levels naturally. Future study should take into account the numerous variations between human and mouse stomach tissue, as well as the necessity to make GINS cells more resistant to immune system attack.
However, early indications are encouraging. The study strengthens a variety of approaches being investigated by scientists to treat diabetes, including dietary changes and adjustments to how insulin is absorbed by the body.
This is a proof-of-concept study that provides us with a strong framework for creating a treatment for type 1 diabetes and severe type 2 diabetes based on patients' own cells, adds Zhou.
The ultimate goal of the research is to create a method that would allow for the relatively simple extraction of stomach stem cells from patients, followed by the transplantation of insulin-secreting organoids that could control blood sugar levels without the need for further medication, many weeks later.




Comments
Post a Comment
Share your views